enhanced First Trimester Screening (eFTS) Guide
Enhanced First Trimester Screening (eFTS) is a screening test for trisomy 21 and trisomy 18, consisting of a nuchal translucency ultrasound and bloodwork in the first trimester of pregnancy. This test is the preferred multiple marker screening modality.
Step-by-step instructions are outlined below, to provide guidance to health-care practitioner for how to order eFTS in Ontario.
Step 1 |
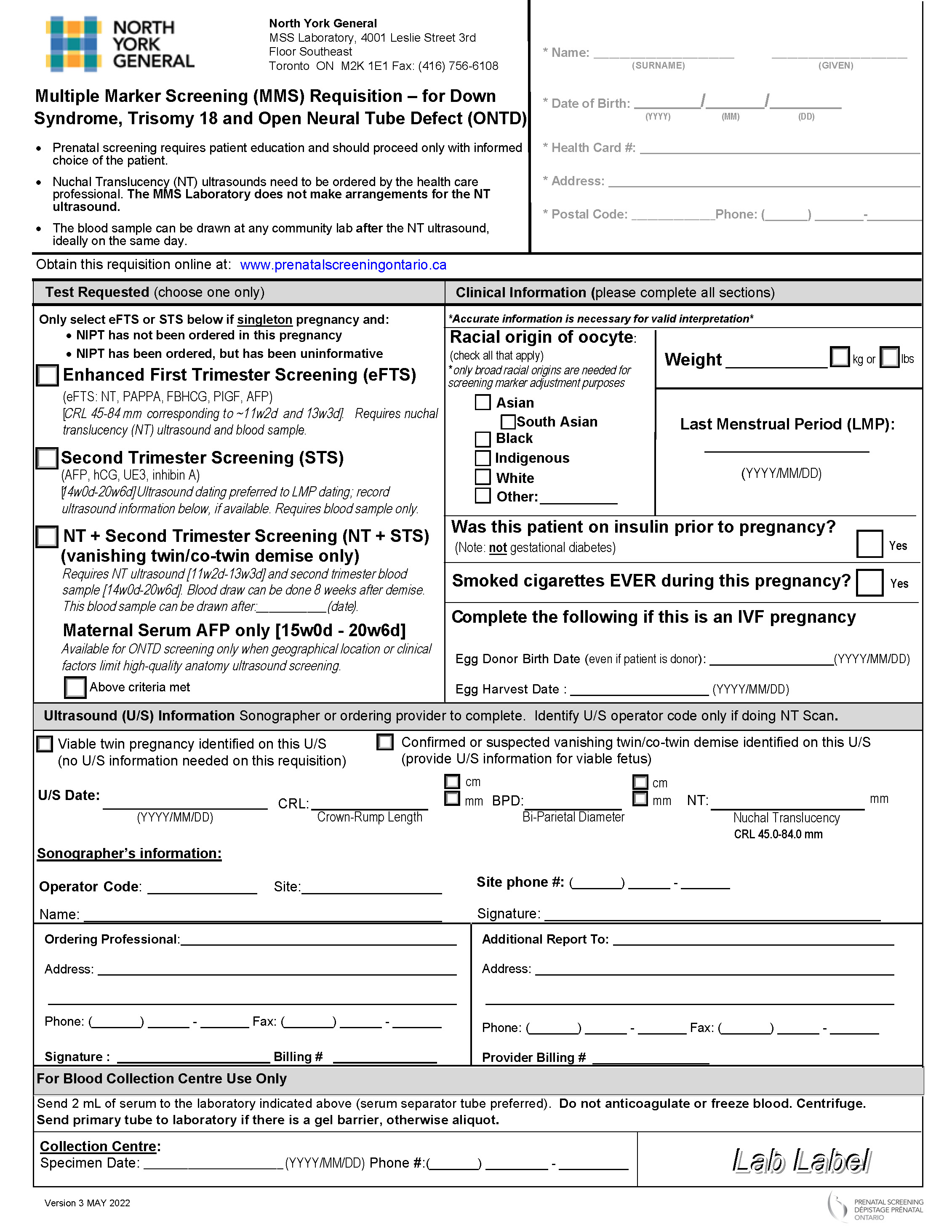
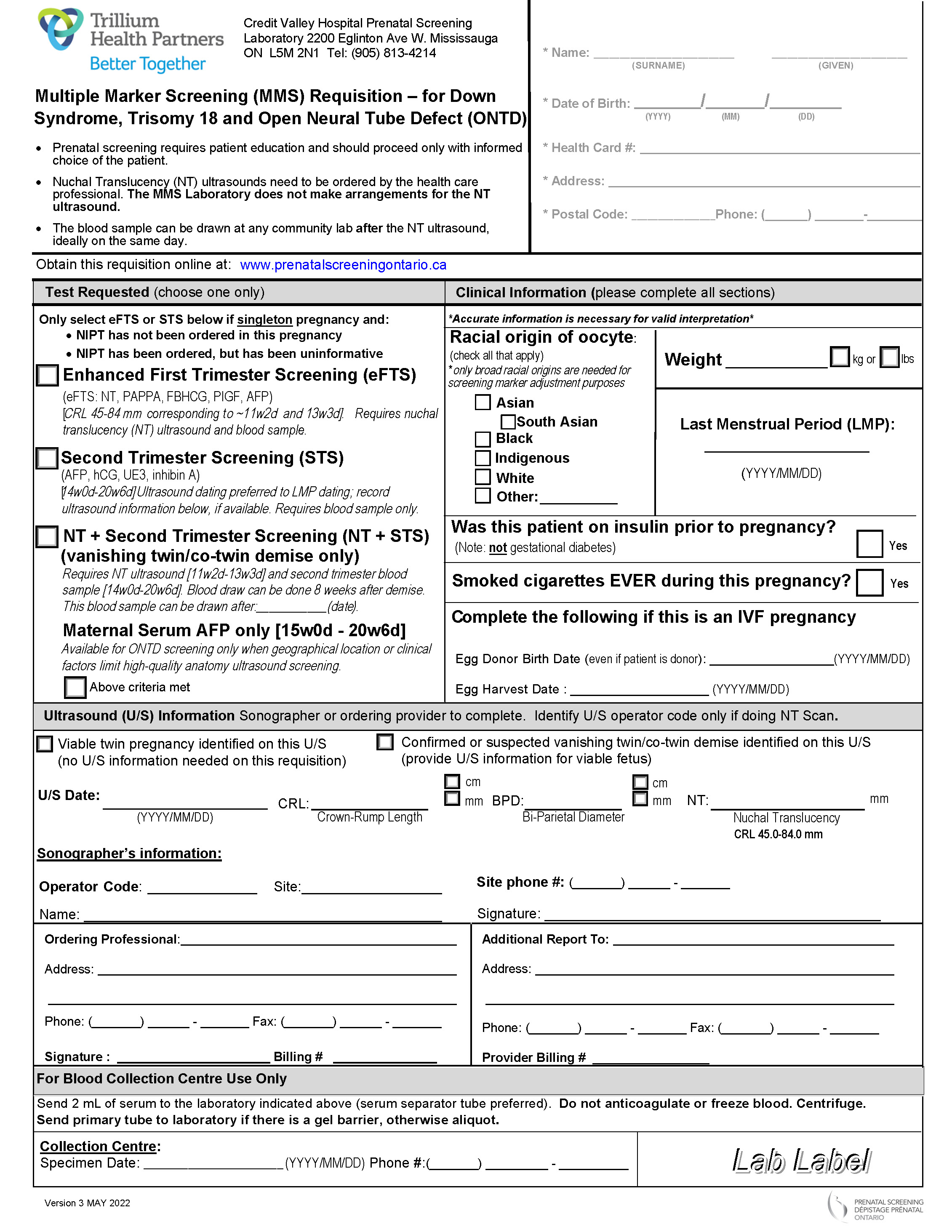
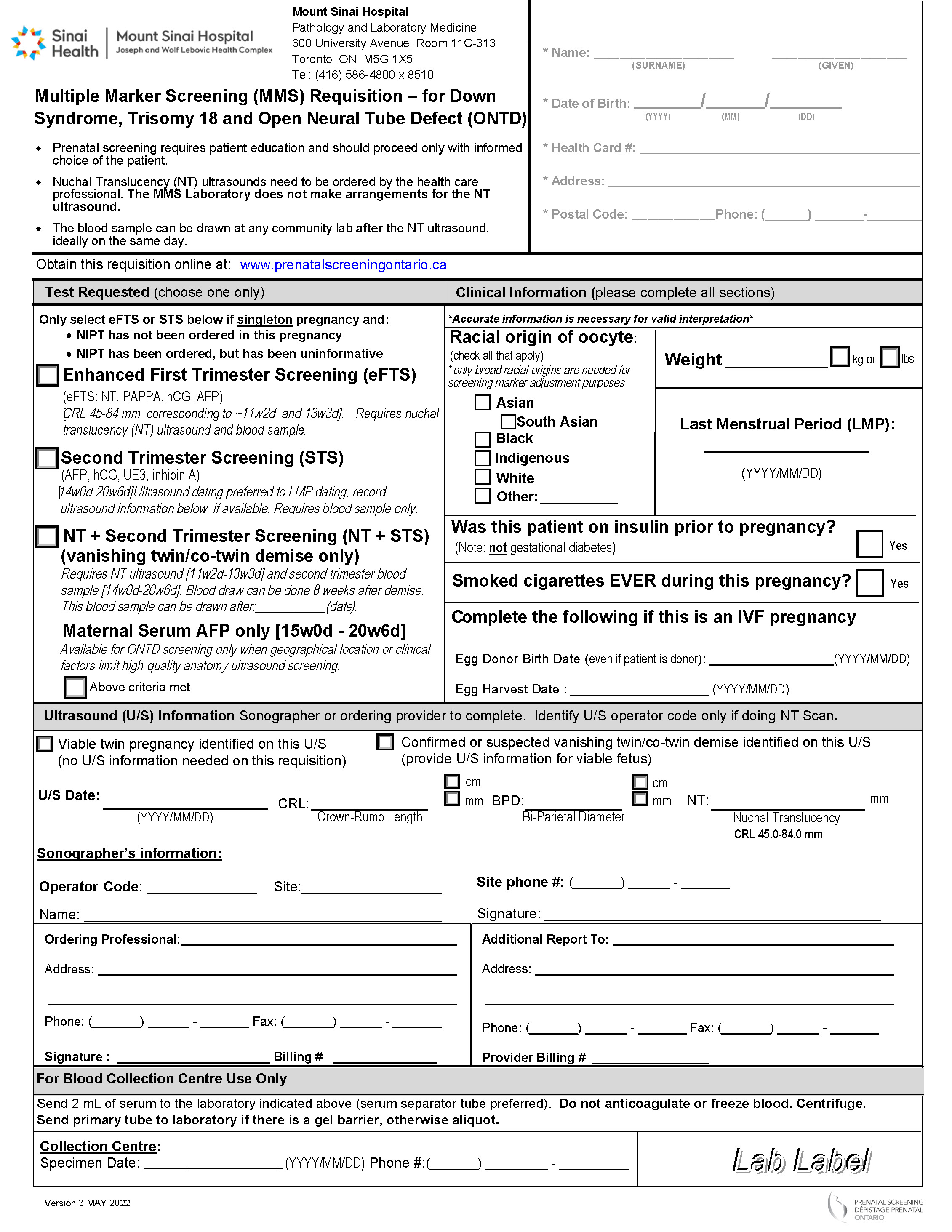
Complete the Multiple Marker Screening Requisition
Multiple Marker Screening (MMS) is done by 3 provincial laboratories: Trillium Health Partners - Credit Valley Hospital, Mount Sinai Hospital and North York General Hospital. Check out our interactive map to learn which of the three requisitions you should use.
The Multiple Marker Screening Requisition must be filled out in full prior to the NT ultrasound. Please note that missing information decreases the quality of the screen and can potentially delay the results.
Demographics Section
The pregnant individual’s name, date of birth, health card number, address, and phone number should be completed.
"Test Requested" Section
Check off the enhanced First Trimester Screening (eFTS) option only for:
- Singleton pregnancies. eFTS cannot be done for twin pregnancies. If you are aware of a twin pregnancy prior to filling out this requisition, offer OHIP-funded NIPT instead.
- Pregnancies without a vanishing twin/co-twin demise. If you are aware of a vanishing twin scenario prior to filling out this requisition, order "NT + Second Trimester Screening”.
-
Pregnancies under 13 weeks 3 days gestation. eFTS is available when the crown-rump length measurement (the measurement of the length of embryo from top of the head to the bottom of the torso) at the time of NT ultrasound is between 45 and 84 mm. This corresponds to a gestation between 11 weeks 2 days to 13 weeks 3 days gestation1.
-
Pregnancies for which NIPT has not been ordered.
-
Pregnancies for which NIPT has been ordered, but has been uninformative.
|
1The Multiple Marker Screening labs determine the gestational age based on the published tables of Hadlock and Daya. |
|
"Clinical Information" Section
Accurate and complete information in this section will increase the quality of the screening results by reducing the chance of false positives and false negatives.
I have some questions about you to ask to make sure your screening is as accurate as possible.
| Racial Origin |
|
Indicate the racial origin of the pregnant individual. Racial origin information is needed because the concentrations of screening markers have been shown to vary depending on the racial origin. Therefore, a pregnant individual’s screening markers are adjusted based on the racial origin information provided. Only the broad racial origins listed are needed for screening marker adjustment. The categories on this requisition are not inclusive of all the race categories commonly used as social descriptors in Ontario. Description / examples for each of the racial origin categories on the requisition:
Racial origin should be as accurate as possible and should reflect the individual’s ancestral background (which may or may not align with how the pregnant individual identifies), not simply their birth country. This information should be obtained directly from the pregnant individual whenever possible.
|
| Weight |
|
Indicate the pregnant individual’s weight, including units (pounds (lbs) versus kilograms (kg)), at the time when this requisition is completed. This information is used for screening marker adjustments. Ensure the weight that you document is accurate. A weight discrepancy of 10 or more pounds (4.6 kilograms) has a significant impact on the risk for trisomy 21 for pregnant individuals with a risk close to the screening cut-off.
|
| Last Menstrual Period |
|
The Last Menstrual Period (LMP) is not needed for eFTS. The crown-rump length measurement at the time of NT ultrasound is used instead of the LMP to establish the gestational age of the fetus. |
| Insulin-Dependent Diabetes Mellitus History |
|
Indicate if insulin-dependent Diabetes Mellitus was diagnosed prior to the individual’s current pregnancy. Individuals with insulin-dependent Diabetes Mellitus have been shown to have different concentrations of screening markers compared to those who do not have this diagnosis. Screening marker adjustments must be made to account for these differences. No screening marker adjustments are made for pregnant individuals with a history of gestational diabetes or preexisting diabetes that is not managed with insulin.
|
| Cigarette Smoking / Vaping History |
|
Indicate if the pregnant individual has smoked or vaped any amount of nicotine at any point in the current pregnancy. Individuals with a history of smoking or vaping nicotine have been shown to have different concentrations of screening markers compared to those who do not have this history. Screening marker adjustments must be made to account for these differences. If the requisition does not include information about the smoking or vaping history, the pregnant individual is considered a non-smoker. Due to lack of published data, pregnant individuals exposed to second-hand smoke are considered non-smokers.
|
| In Vitro Fertilization (IVF) History |
|
If the pregnancy was conceived using in vitro fertilization (IVF), indicate the egg harvest date and date of birth of the egg donor (either self or non-self). If the egg donor's full date of birth is unknown, indicate the year of birth. If only the year of the donor date of birth is provided, July 1 of the provided year is used as the date. This information is requested because the age of the egg at the date of delivery influences the enhanced First Trimester Screening risk. In addition, screening marker levels vary between IVF and natural conceptions, and screening marker adjustments must be made to account for these differences.
|
"Ultrasound Information" Section
Be aware that only the sonographer / physician performing the NT scan completes the "Ultrasound Information" section when ordering eFTS.
| If a suspected or confirmed vanishing twin/co-twin demise is identified on the NT ultrasound |
|
If a suspected or confirmed vanishing twin/co-twin demise is identified on the NT ultrasound, the sonographer / physician performing the scan checks off “Confirmed or suspected vanishing twin/co-twin demise identified on this U/S” in this section. Checking this box signifies to the MMS lab that NT + STS needs to be performed. The pregnant individual is to proceed with the blood draw, and upon receipt of the blood sample, the MMS lab notifies you of the next steps, which would be to arrange an STS blood draw between 14 weeks 0 days to 20 weeks 6 days (and 8 weeks after the estimated date of demise). |
| If a twin pregnancy is identified on the NT ultrasound |
|
If a twin pregnancy is identified on the NT ultrasound, the sonographer / physician performing the scan checks off “Viable twin pregnancy identified on this U/S” in this section. Checking off this box signifies to the MMS lab that this is a twin pregnancy, therefore eFTS cannot be performed. The pregnant individual is to proceed with the blood draw, and upon receipt of the blood sample, the MMS lab notifies you that First Trimester Screening for twin pregnancies has been discontinued in Ontario and that OHIP-funded NIPT should be ordered instead. |
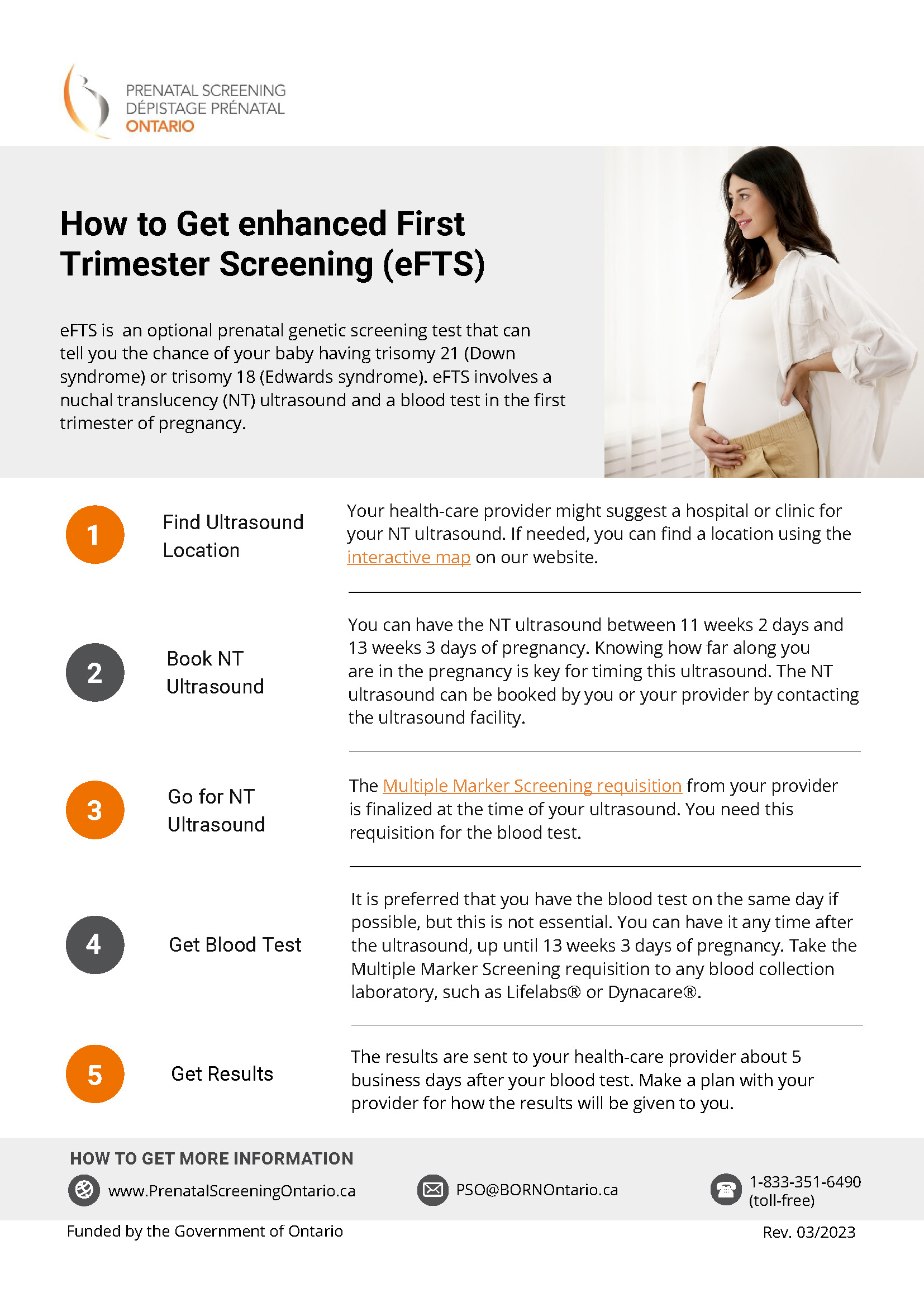
Step 2 |
Complete a Nuchal Translucency Ultrasound Requisition
Visit our interactive map to find facilities offering NT ultrasound in Ontario. You can contact the ultrasound facility of interest to obtain the centre-specific ultrasound requisition

Step 3 |
Provide Requisitions to the Pregnant Individual
- Give both the completed NT ultrasound requisition and Multiple Marker Screening requisition to the pregnant individual.
- If your office is booking the NT ultrasound, it is helpful to fax the MMS requisition with the ultrasound requisition to the ultrasound facility. It is important that the ultrasound facility has both of these requisitions at the time of the ultrasound appointment, either from your office or from the pregnant individual.
- Check if additional requisitions are required by the ultrasound and blood work facilities, such as the Ministry of Health and Long Term Care Laboratory Requisition.

Step 4 |
Provide Step-by-Step Instructions to the Pregnant Individual
- Provide clear instructions to pregnant individual for how to navigate the steps involved in obtaining enhanced First Trimester Screening, as outlined in the leaflet. Please note that Prenatal Screening Ontario does not organize prenatal genetic screening tests, such as the NT ultrasound.
- If the pregnant individual goes for the NT ultrasound but the bloodwork is not done prior to 13 weeks 3 days gestation, eFTS may not be possible for them. Contact Prenatal Screening Ontario or the Multiple Marker Screening Laboratory to learn about which screening options are possible.
Step 5 |
Obtain Report and Check for Accuracy
- Results are reported to you by the MMS lab generally within 5 business days. It is important to take into account the time lag that can occur between the time when the report is ready and when it is received by your office.
- If you do not receive the prenatal screening report, we encourage you to follow up with the MMS lab directly. Prenatal Screening Ontario does not have access to screening results of individuals.
- Review the screening report for accuracy. If any errors or omissions are noted, contact the MMS Laboratory to determine if an amendment to the report is needed.
When is a Report Amended?
A report is considered “amended” if changes are made after the report has been issued to the health-care practitioner. Amending reports is necessary to correct errors that include data being inaccurately provided on the requisition. Some examples are inaccurate racial origin identification, inaccurate diabetes status, and correction of weight, due to either wrong units (i.e. pounds or kilograms) or difference in weight of more than 5 - 10 pounds (2.3 - 4.6 kilograms)1 from that given on the requisition.
1North York General Hospital and Mount Sinai Hospital labs will amend a report if there is a difference in weight of more than 10 pounds. The Trillium Health Partners lab will amend a report if there is a difference in weight of more than 5 pounds.
How is a Report Amended?
Health-care practitioners can write the amendment(s) directly on the screening report and fax it back to the Multiple Marker Screening Laboratory, indicating that an amendment is required as per the enclosed report. Alternatively, health-care practitioners can fax a note with the pregnant individual's name, date of birth, health card number, and details related to the amendment request, including relevant clinical information.
Step 6 |
Communicate Results and Next Steps
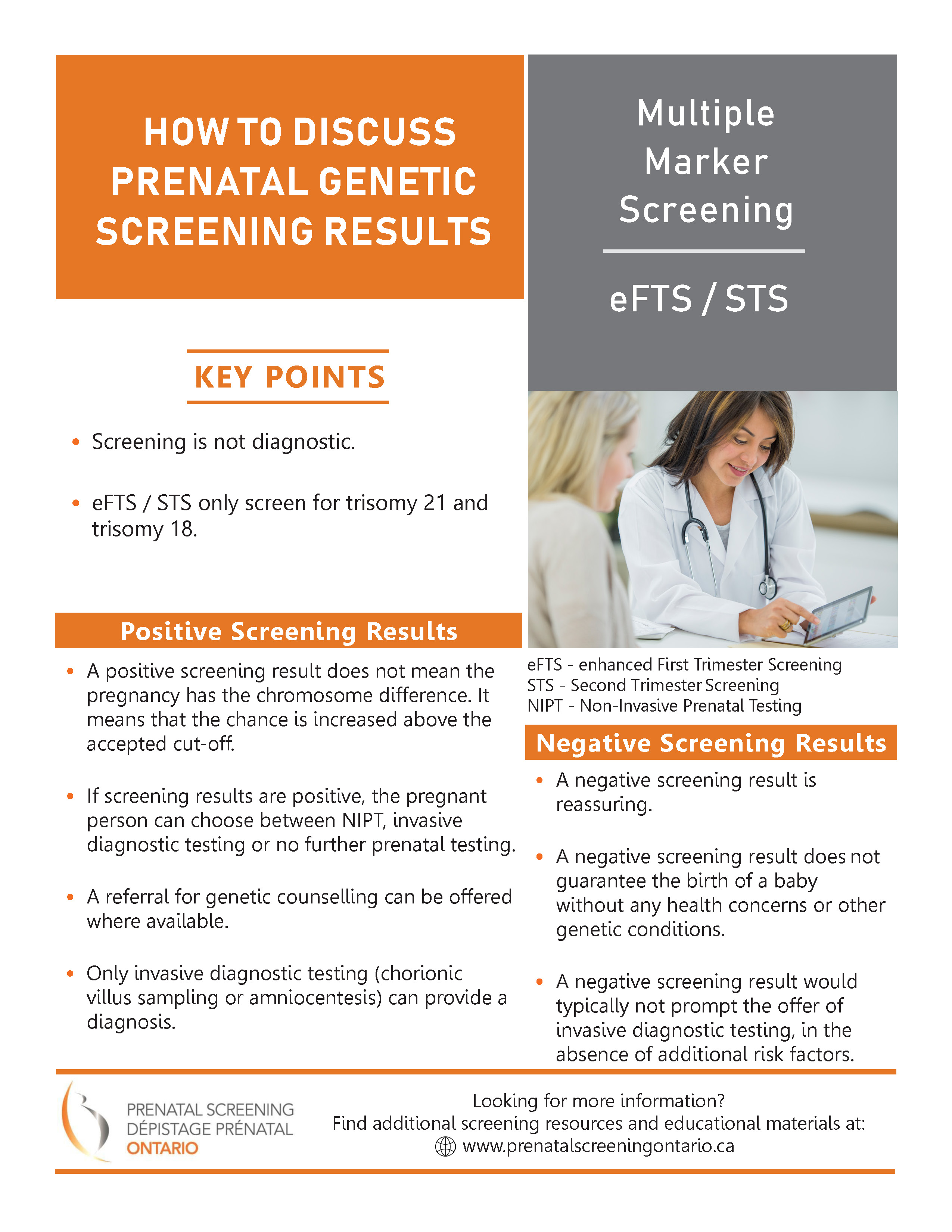
- Once the report is received, results should be communicated in both “screen positive” and “screen negative” scenarios, including the specific risk estimate provided on the report.
- Ensure continuity of care: forward the report to any other practitioners involved in the care of the pregnant individual.
The results of the nuchal translucency ultrasound will be sent separately by the ultrasound facility. If the nuchal translucency measurement is increased (3.5 mm or above), inform the pregnant individual of this result as soon as possible and offer a referral for genetic counselling irrespective of the eFTS results


 Subscribe to this page
Subscribe to this page